Contractual Tendon Release: The Truth You Need to Know

If you hear the words 'contractual tendon release' and picture a scary, risky surgery, you’re not alone. Most people imagine it’s only for severe injuries or athletes, but actually, this procedure can show up in regular folks’ lives too—like people dealing with tight fingers or stiff ankles that make everyday stuff a struggle.
The basics? This surgery helps free a tendon that’s become too tight, often due to scarring, injury, or conditions like cerebral palsy. Instead of letting that stiffness run your life, a doctor can literally release the pressure by cutting or lengthening the tendon. This can mean less pain, better movement, and an easier time with day-to-day tasks.
But is it for everyone? Nope. It’s usually done when therapy, splints, or other less invasive fixes can’t get the job done. If you’re on the fence, there are clear signs and symptoms to watch for, plus some real-life questions your doctor should answer before you make any big decisions. Stick around—you're about to get some straightforward answers and smart advice that most clinics won’t mention until you’re already in a gown.
- What Is Contractual Tendon Release?
- Who Actually Needs This Surgery?
- What Happens During the Procedure?
- Recovery: The Real Story
- Risks and What Can Go Wrong
- Smart Tips Before You Say Yes
What Is Contractual Tendon Release?
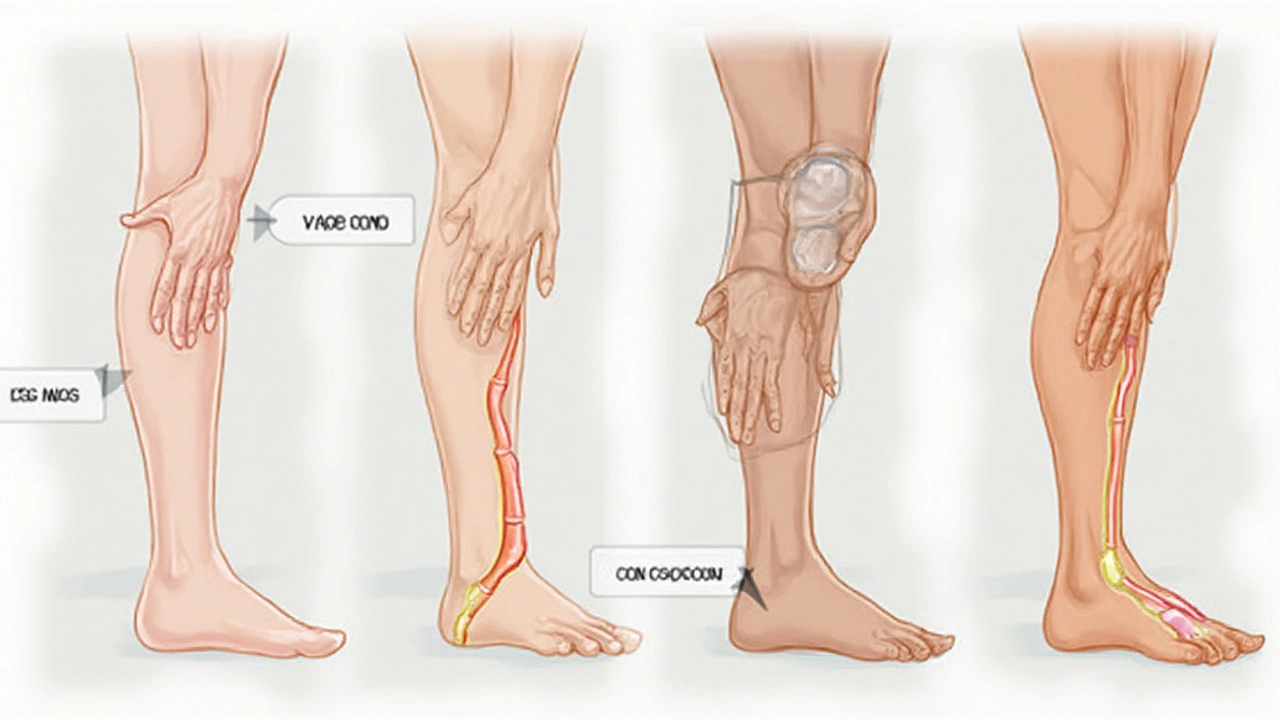
Let’s break down what happens when doctors talk about contractual tendon release. It’s a surgical procedure used when a tendon gets stuck or too tight, often from an old injury, scarring, or a health condition that messes with your muscles. Basically, tendons are the thick cords that connect muscle to bone, and when they get too short, stiff, or locked up, your joint can’t move well. This is called a contracture. It can mess with your ability to walk, open your hand, or even stand up straight.
The surgery works by lengthening or releasing the tendon. Sometimes, the tendon is simply cut to loosen it up, while other times, doctors might remove a small section or reposition it where it won’t pull so tightly. It’s common in folks with cerebral palsy, stroke damage, or injuries that heal with a lot of scar tissue.
You might be surprised, but this is one of the go-to treatments when physical therapy, stretching, or splinting just can’t fix things. Here are the key situations where doctors usually recommend it:
- Finger contractures (like in Dupuytren’s contracture or trigger finger)
- Clubfoot in kids
- Achilles tendon issues that cause walking problems
- Major scarring from burns or accidents
- Long-term muscle tightness after a stroke
How common is it? According to recent hospital stats in the U.S., over 14,000 tendon release surgeries happen every year, just for hand and wrist cases. That doesn’t even include kids with clubfoot or adults with ankle contractures. Here’s a quick look at the numbers:
| Condition | Approx. Annual Procedures (U.S.) |
|---|---|
| Hand/Wrist Contractures | 14,000 |
| Clubfoot | 6,000 |
| Achilles Contractures | 3,500 |
This means you’re far from alone if the word “release” comes up in your doctor’s office. What matters most is what happens before and after the procedure—which can make all the difference in your recovery.
Who Actually Needs This Surgery?
Not everyone with a stiff joint or tight tendon should jump straight into surgery. Contractual tendon release is meant for people whose tendons have tightened up so much that moving a finger, foot, or elbow is tough or even impossible. We’re talking about everyday actions that people simply can't do anymore—stuff like holding a coffee mug, walking flat-footed, or buttoning a shirt.
This kind of surgery pops up most often for these groups:
- Kids and adults with cerebral palsy. Their muscles and tendons can tighten from a young age, making it hard to walk or use their hands.
- People with Dupuytren’s contracture. This causes the fingers—usually the ring and pinky—to curl toward the palm and get stuck.
- Stroke survivors. Strokes can mess with nerves and lead to tight, curled-in limbs.
- Folks recovering from bad injuries or burns. Scars form, tendons shorten, and suddenly you can’t fully stretch out that joint anymore.
But doctors don’t just hand out these surgeries to anyone. First, they try other treatments—think physical therapy, splints, or even meds to relax the area. Surgery becomes the go-to when these options just aren’t cutting it, and life is still on pause.
| Condition | Likelihood of Needing Surgery |
|---|---|
| Cerebral palsy (kids) | Up to 40% after therapy fails |
| Dupuytren’s contracture | About 20% of advanced cases |
| Post-burn contractures | Roughly 30% with severe scarring |
| Stroke contractures | Varies, but higher if rehab doesn't help |
If a person has tried months of therapy and still can't use their hand, lift their foot, or straighten their leg, that's when doctors start talking surgery. It’s not first choice—it’s the last tool in the toolbox when nothing else gets results.
Bottom line: if your day-to-day is held hostage by a tight tendon and you’ve given everything else an honest shot, it may be time to chat about this procedure. But it’s a step-by-step decision, not a snap judgment.
What Happens During the Procedure?
So, you’ve made the choice to go ahead with a contractual tendon release. Here’s what actually goes on in that operating room—minus the sugarcoating.
First off, the type of anesthesia depends on the body part and your doctor’s call. For fingers or the hand, you’ll usually just get a local numbing shot. For larger tendons (like in your leg), you might get general anesthesia or something that keeps you relaxed but awake, called sedation.
- Incision: The surgeon makes a small cut right over the tight or contracted tendon.
- Release: Using special tools, they either snip or split the tendon, or sometimes they stretch and lengthen it by making small cuts (that’s called Z-lengthening if you want the fancy term).
- Check movement: The doctor moves your finger, foot, or whatever joint to check right there if the tendon is now looser and lets you move better.
- Closing up: They stitch you up, put on a little bandage, and sometimes add a splint or soft cast to keep things in shape while you heal.
The whole thing might only take 30–60 minutes for something like a finger. If it’s a bigger area, it can run a bit longer. And you’re usually home the same day.
| Fact | Details |
|---|---|
| Main Purpose | Loosen tight tendon for better movement |
| Anesthesia Types | Local, regional, or general |
| Avg. Time in OR | 30 to 90 minutes |
| Hospital Stay | Usually go home same day |
| Common Uses | Fingers, feet, elbows, sometimes hamstrings |
Here’s a tip: ask your surgeon if the procedure will be "open" (meaning a cut you can see) or "percutaneous" (tiny poke holes and less scarring). The second option sometimes means a faster recovery. Also, your surgeon should talk you through what the release will really change for your daily life, so you know what to expect and aren’t surprised later.
Recovery: The Real Story
So, what really happens after a contractual tendon release? Most folks think they'll be back to normal in a few days, but it usually takes longer. Right after surgery, you’ll probably feel sore and a bit stiff. Swelling and some bruising are pretty common. Your doctor might send you home the same day, especially if it’s a smaller tendon. But don’t expect to drive yourself—get a ride.
The main thing after surgery is rest and protection. The area will usually be wrapped or put in a splint to keep things stable. This isn’t just for comfort—it’s to help the tendon heal the right way. Follow those instructions even if you’re itching to take the wrap off early. Most people wear the splint for anywhere from a week to several weeks, depending on how deep or complicated the release was.
Physical therapy usually starts soon—sometimes within days. It’s not just busywork. If you skip those exercises, you risk the tendon getting tight again. Therapists will show you simple moves to keep the joint flexible and rebuild strength. It doesn’t feel glamorous, but sticking with therapy helps you actually get back to using your hand, foot, or whatever part you had fixed.
- Expect full recovery to take anywhere from a month to a few months, depending on the joint, your age, and other health stuff.
- Ice, elevation, and medication (if needed) will help with pain in the early stages.
- Watch for signs of infection—redness, heat, or weird drainage—and call your doc if anything looks off.
Some people can do household tasks within a week, others need help for longer. Don’t rush it or you’ll just slow things down. Stick with your follow-ups. Your doctor will want to see that the tendon isn’t getting tight again and that your range of motion is actually improving.
Bottom line: Be patient, ask questions, and don’t bail on therapy. Recovery isn’t instant, but it can make a huge difference if you put in the effort.
Risks and What Can Go Wrong
No surgery is perfect, and contractual tendon release is no exception—even when done by the best surgeons. Before you sign any forms, it’s smart to know what you might be up against. The risks aren’t just from the knife; recovery has its own pitfalls.
Here’s what the research and doctors actually talk about once you start asking real questions:
- Infection: Even with careful cleaning and antibiotics, any cut can get infected. Symptoms might be more swelling, redness, or pus days after surgery.
- Nerve injury: There are a lot of nerves running near tendons. Sometimes, surgery can nick a nerve, causing numbness, tingling, or even loss of feeling. Some folks recover in weeks, while others never get full sensation back.
- Recurrence: Think the problem is 100% gone? Not always. About 10-30% of people with certain kinds of contractures (like Dupuytren’s) see the stiffness or tightness return within a few years.
- Scarring or stiffness: Ironically, the fix can sometimes make you trade old problems for new ones. Scarring from the incision or the body’s healing response can actually make tissues stiff again, so regular rehab is key.
- Slow healing: Some people heal at a snail’s pace, especially if they have diabetes, are smokers, or are older. That means more follow-ups and longer time away from daily routines.
- Excessive swelling or blood clots: Not common, but can happen, especially in leg surgeries. Watch for swollen, hot, or painful limbs during recovery.
Here’s a quick look at some numbers that might help make sense of it:
| Risk | Chance (% of cases) | Notes |
|---|---|---|
| Infection | 1-5% | Mostly mild, but can delay healing |
| Nerve Injury | 2-8% | Usually temporary, but not always |
| Recurrence | 10-30% | Higher in hand contractures like Dupuytren’s |
| Scarring/Stiffness | Up to 15% | More likely without good rehab |
An honest tip: ask your surgeon how many of these surgeries they’ve done and how often their patients run into any of these problems. The best ones won’t dodge the question.
Smart Tips Before You Say Yes
Saying yes to any surgery is a big decision. Contractual tendon release isn’t something you just schedule on a whim. Here’s what you really need to think about before you sign those papers.
- Get a second opinion. Not every doctor thinks alike, and you want to be sure this is the best route. Sometimes other treatments work just as well if not better for your specific situation.
- Ask what success looks like. Some folks expect miracles, but results can vary. Straight talk: about 70-80% of people with hand contractures from Dupuytren’s disease, for example, see better movement after release. Still, that leaves a chunk who might not notice a huge difference.
- Clarify the recovery time. Some tendon releases let you return to daily stuff in a week or two, but bigger fixes can mean months of therapy. Double-check what’s normal for your specific tendon.
- Get upfront about all the risks. There’s a small chance of infection—studies list infection rates around 1-3% depending on the procedure and hospital. Nerve damage or less movement than you hoped can also happen, so press for real numbers (not just "rare" or "unlikely").
- Check insurance and costs. Some policies count this as elective, which could mean more out-of-pocket. Don’t assume everything will be covered—get written estimates when possible.
- Talk through aftercare resources. Physical therapy isn’t optional for most people—it’s non-negotiable for a decent outcome. Ask who sets that up and what’s included.
Here’s a quick peek at how things usually stack up for contractual tendon release patients compared to non-surgical options:
| Option | Average Recovery | Improvement Rate | Main Risks |
|---|---|---|---|
| Tendon Release Surgery | 2-12 weeks | 70-80% | Infection (1-3%), Nerve injury |
| Physical Therapy | Ongoing | 40-60% | Minimal (strain, fatigue) |
| Injections/Splints | 1-6 weeks | 30-50% | Skin irritation, tendon rupture (rare) |
Bottom line? Take your time, ask real questions, and don’t let anyone rush you. Decisions about your body and your movement deserve careful thinking and honest answers.





